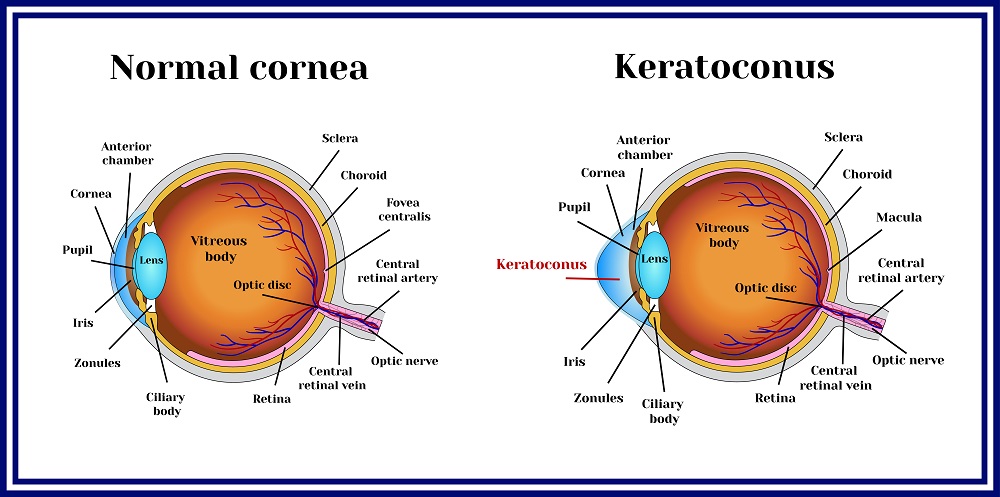
The cornea is the transparent layer that covers the front of the eye and helps in regulating light entering the eye. A healthy cornea promotes clear sight without the use of assistive equipment like glasses and contact lenses.
Corneal ectasia refers to the group of irregularities in the cornea that affects the quality of sight and vision. This condition is usually due to the thinning layer of corneal tissue that eventually leads to the structural change of the cornea into a cone or globular form.
Causes of Corneal Ectasia
Corneal ectasia can be caused genetically, iatrogenically, or through the development of eye illnesses. Some people are genetically born with thinner corneas. This makes them susceptible to developing corneal ectasia during puberty.
Some people are also more susceptible to developing keratoconus especially when genetic components such as subpar vision and irregular astigmatism are present.
Corneal ectasia can manifest during puberty and persist and even worsen as the individual reaches adulthood. When left untreated, this can lead to permanent eye damage and total loss of sight.
Corneal ectasia is not readily identifiable in terms of appearance and will only manifest through mild irregularities in detection skills due to sight disturbances. However, it induces changes in the corneal topography and creates structural imbalances in the cornea.
Eye Illnesses That Contribute to Corneal Ectasia
Eye illnesses that can contribute to the development of corneal ectasia are Pellucid Marginal Degeneration and Keratoglobus.
Pellucid Marginal Degeneration refers to the thinning of the peripheral sections of the cornea. This can lead to the development of the disease of the connective tissues known as the Ehlers-Danlos Syndrome and eventually Keratoglobus or degenerative disease that causes the cornea to assume a globular rather than a curved shape.
Iatrogenic causes refer to the medically induced type of corneal ectasia. Some eye correcting procedures like Laser-Assisted In Situ Keratomileusis (LASIK surgery), Photorefractive Keratectomy (PRK), and Small Incision Lenticule Extraction (SMILE) can eventually cause corneal ectasia due to excessive thinning of the cornea. Contact lenses can also cause corneal warping, which can develop into corneal ectasia when untreated.
Iatrogenic corneal ectasia can manifest through post-operative blurry and fluctuating vision, glare and halos when in direct contact with light, and worsening signs of astigmatism.
Some of the associated risk factors for the development of corneal ectasia are the thickness of the cornea and moderate to severe cases of myopia or nearsightedness. People with thin corneas and myopia are more susceptible to developing corneal ectasia after undergoing invasive procedures.
Diagnosing Corneal Ectasia
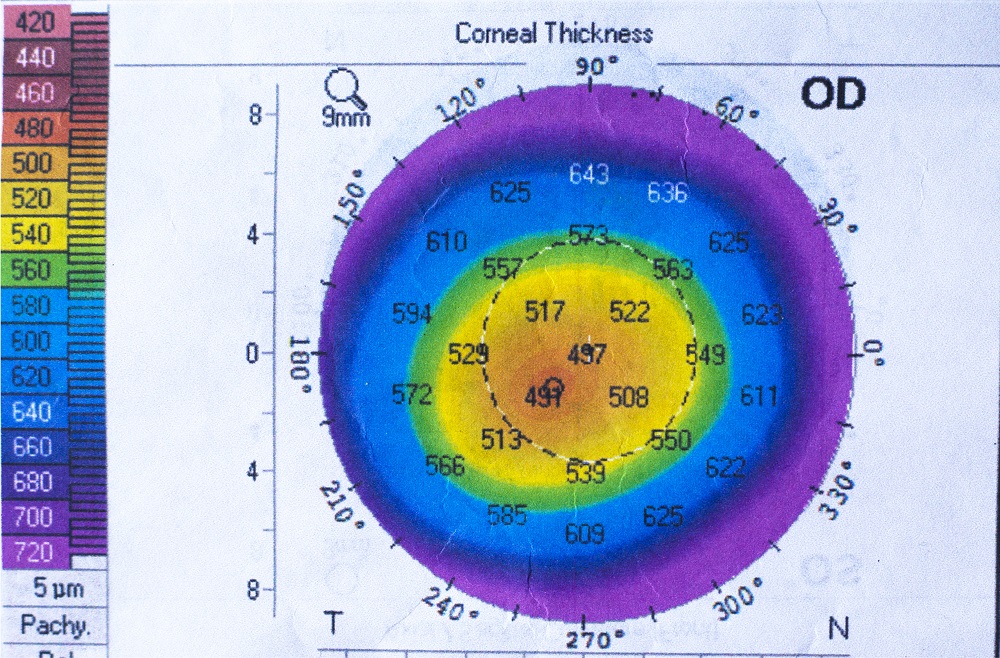
The diagnosis for corneal ectasia depends primarily on the severity of the condition. Moderate and severe corneal ectasia can be diagnosed using a retinoscope, biomicroscopy, and placido disc-based corneal topography.
Corneal topography used to be the standard for diagnosing corneal ectasia due to its capability for determining signs of corneal steepening that can lead to keratoconus and keratoglobus.
With the advancements in technology, corneal tomography is now able to diagnose corneal ectasia at its early stages. Corneal tomography refers to the 3D imaging of the cornea using Slit Scanning, Very High Frequency (VHF) Ultrasound Imaging, and Scheimpflug Imaging.
Slit Scanning provides a 3D topographical mapping of the edges of the cornea. Scheimpflug Imaging uses a pentacam or oculus in analyzing the corneal surface. The VHF Ultrasound measures the thickness of the cornea. These procedures determine various dimensions of the cornea and assess its structural integrity before undergoing operative procedures.
Corneal hysteresis is another new diagnostic procedure that alters the traditional means of assessing the cornea using its thickness and shape. This procedure measures the viscosity and elasticity of the cornea and evaluates its capacity to respond to visual cues.
Corneal Ectasia Treatment Procedures
Corneal ectasia has both invasive and non-invasive treatment. Mild severity of the condition can be treated non-invasively using glasses and contact lenses.
Hybrid contact lenses help improve the condition while also promoting comfort. The most effective contact lens for improving irregular corneal structure is the rigid gas permeable (GP) contact lenses. This is usually the most recommended treatment for mild cases of corneal ectasia.
Scleral lenses and Intacs are also non-surgical and non-invasive treatments for mild corneal ectasia. Scleral lenses help in covering the entire cornea to prevent structural change. Usually, these lenses are used post-operative as the person is recovering from LASIK surgery.
Intacs are semi-circular structures inserted into the cornea to stop the structural change of the cornea or to prevent the development of corneal ectasia conditions.
Surgical and invasive procedures, however, offer more permanent solutions to corneal ectasia, especially the moderate and severe cases. Corneal transplant is one of the oldest surgical procedures for treating corneal ectasia. This procedure involves penetrating keratoplasty where the surgeons remove the abnormal parts of the cornea, replace them with a donor cornea, and then secure the new cornea with stitching. This requires 12 months of close monitoring for any potential complications.
While Photorefractive Keratectomy (PKP) can also help remedy corneal ectasia, Deep Anterior Lamellar Keratoplasty (DALK) is a safer procedure with a lower chance of graft rejection. DALK involves removing the corneal stroma until the Descemet’s Membrane and replacing it with a donor cornea. This procedure promotes better healing and little loss in the endothelial cells.
Intrastromal Corneal Ring Segment Implantation is a procedure used for moderate types of corneal ectasia. This is most effective when there is only mild corneal scarring. This procedure involves inserting up to two polymethyl methacrylates into the interior of the corneal stroma to regulate its shape and prevent steepening.
Corneal crosslinking (CVL) is also another form of corneal ectasia treatment. This involves applying vitamin B2 or riboflavin on the eye using a solution and activating it using UV light. This procedure can be performed with or without the epithelial layer.
This procedure helps in increasing the integrity of the cornea and promotes forming newer and better bonds with the collagen in the corneal stroma. This will help improve visual performance and slow down or halt the progression of corneal ectasia.